37 year old male with abdominal pain
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current based inputs.
M Rambai ,9th semester
Roll number 78
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE
37 yr Old Male Auto Driver By Occupation Came to Casualty with C/o Pain abdomen since since 6 days
HOPI :-
Patient Was Apparently Asymptomatic Till yesterday Night Then he developed pain abdomen At 1 AM after Passing Stools, After Waking Up From The Bed
Then The Pain Was Gradually Increased to Severity in The Morning 6 AM , which was Squeezing Type Radiating To the Back
Patient also had Vomitings ( 3 Episodes in A Day ) with food Particles As Content , Non Bilious , Non Projectile .
Pain Aggravated While Sitting , and Decreased on Sleeping in Right Lateral Position
Patient Also Noticed Pain in the Left hypochondrium and Thought To be Heart Problem and Approached Nearest Cardiologist In Nalgonda . Cardiologist Said , There is No Problem Related to the Heart after doing an ECG and Advised Admission In Some Other Hospital For The Pain The Patient Was Complaining .
The Patient Came To our hospital for Further Treatment .
PAST HISTORY :-
Known case of Hypertension Since 3 months ( Diagnosed In the Government Hospital And Advised To Take Medication , Pateient used Medication for A Week and Then Stopped .)
No Similar complaints In the past .
No H/o DM, TB , Epilepsy , Asthma.
PERSONAL HISTORY:
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and bladder- regular
Addictions - alcohol since 15 years
Gutkha since 15 years
Cigarette since 15 years
Allergies - None
FAMILY HISTORY:
There is no significant family history
TREATMENT HISTORY :
For urinary tract infection 4 years back
GENERAL EXAMINATION :-
Pateint is conscious , coherent , cooperative and well oriented to time,place and person .
Moderately built and moderately nourished.
.
Vitals
Temp - afebrile
BP - 160/100 mm hg
PR - 89 bpm.
RR - 19 cpm
SYSTEMIC EXAMINATION
ABDOMINAL EXAMINATION
INSPECTION:
Shape –slightly distended
Umbilicus – Central, inverted
Flanks – free
Skin- no sinuses, striae are seen
Dilated veins – absent
Movements of the abdominal wall with respiration is present
No visible gastric peristalsis and no visible pulsations.
PALPATION:
No local rise of temperature
And tenderness
All inspectors findings are confirmed.
Deep Palpation- No organomegaly seen
PERCUSSION:
Percussion of Liver for Liver Span
Percussion of Spleen- Dull note in percussion
There is no fluid thrill, shifting dullness
AUSCULTATION:
Bowel sounds are absent
CARDIOVASCULAR SYSTEM -
- S1 , S2 heard
- no murmurs and no thrills
●RESPIRATORY SYSTEM-
-Position of trachea is central
-Bilateral Normal vesicular breath sounds
●CNS-
- higher motor functions are intact and no focal neurological deficits
INVESTIGATIONS
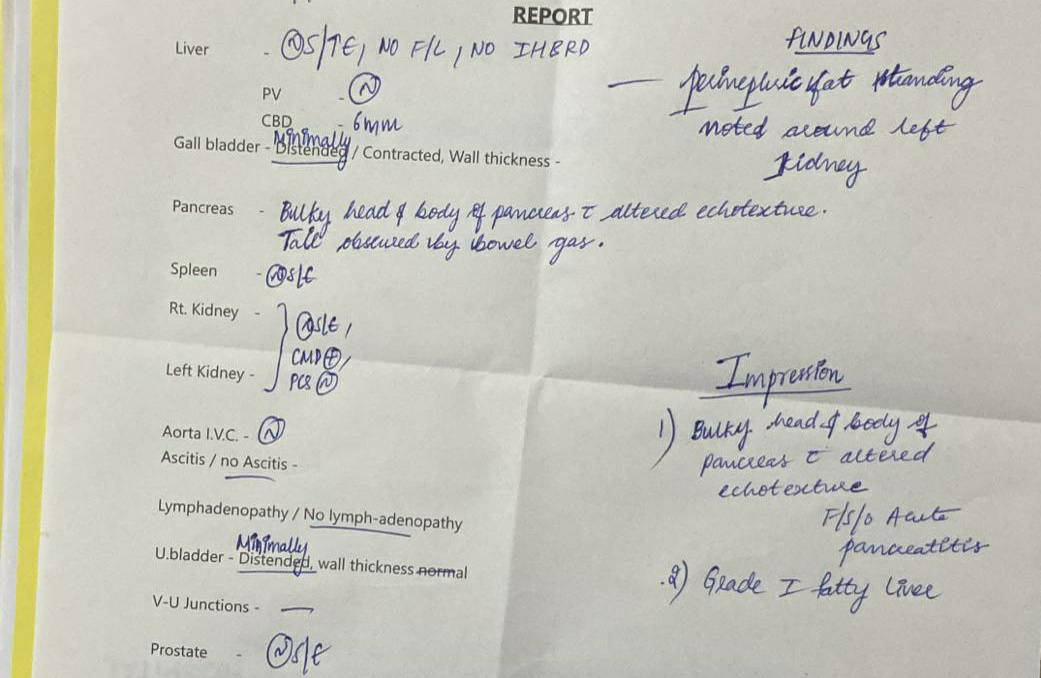
Serum Lipase - 94
Serum Amylase - 268
HAEMOGRAM
Haemoglobin - 19.7
Total Count - 10,700
RBC -
Platelet Count - 2.35
RFT
S Urea - 12
S Creatinine - 0.9
S Calcium - 9.9
Na - 140
K - 3.7
Cl - 98
LFT
Total Bilirubin - 2 .52
Direct Bilirubin - 0.98
Ast - 45
Alt - 34
Alk P - 165
Total Protein - 8.1
Albumin - 4.1
A/G - 1.03
CRP - Positive 2.4 mg/dl
HbA1c - 7.0 %
Serology - Negative
PROVISONAL DIAGNOSIS
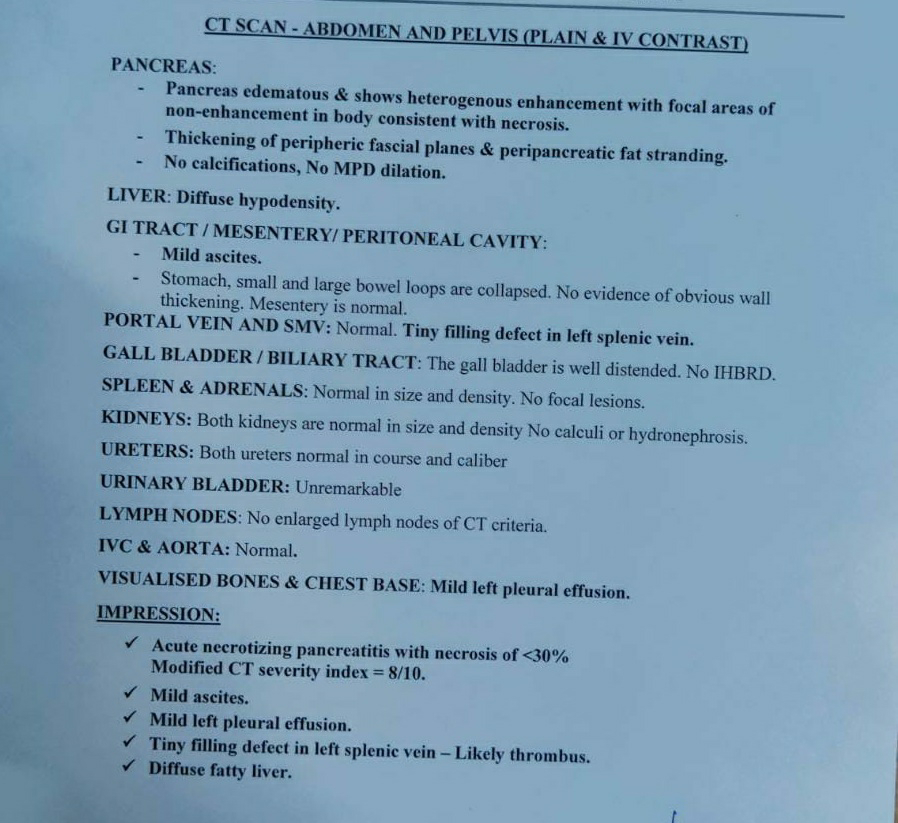
Acute Pancreatitis
Treatment
1. Nbm till further orders.
2. IVF- NS & RL @ 100ml/hr.
3. Inj. Pantop 40mg/IV/OD.
4. Inj. Zofer 4mg/IV/SOS.
5. Inj. Tramadol 1amp in 100 ml/NS/IV/BD.
6. Inj. THIAMINE 2amp in 1 NS/IV/TID.
7. Monitor vitals.





Comments
Post a Comment