50 yr old female with sob and odynophagia
MEDICINE CASE DISCUSSION
March 31,2022.
50 YEAR OLD FEMALE WITH SOB AND ODYNOPHAGIA
Name : Rambai ,9 th semester
Roll no :78
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
CASE
50 Year old , female resident of Hyderabad , homemaker by occupation came to GM opd ,With chief complaints of
* Shortness of breath since 1 month
* Difficulty in swallowing since 3 weeks
* Pedal edema since 1 week
* Chest tightness since 1 week.
TIME LINE OF EVENTS
PAST HISTORY
HYPERTENSION : diagnosed 8years back- taking regular medication
HYPOTHYROIDISM 6years back- taking regular medication(On thyronorm)
Rheumatoid arthritis diagnosed 6 years back(not on medication )
DM type-2 diagnosed 5 months back- not on medication
MILIARY TB diagnosed 1 month back- started on ATT later stopped .
Past clinical images from intern sir
PERSONAL HISTORY
Diet - mixed
Appetite- decreased
Sleep - adequate
No addictions
FAMILY HISTORY
No history of similar complaints in the family
TREATMENT HISTORY
On medication for hypertension
On medication for hypothyroidism
On medication for tuberculosis
Antitubercular treatmentGENERAL EXAMINATION
Patient is concious, coherent and co operative well oriented to time ,place and person.
Patient is examined in a well lit room with adequate exposure, after taking the consent of the patient.
Patient is moderately built and nourished.
VITALS
Temparature: Afebrile
Pulse rate:78 bpm
Respiratory rate: 18 cpm
Blood pressure: 140/80 mm of hg
HEAD TO TOE EXAMINATION
Scalp - hair loss ( alopecia) seen
Eyes - forward protrusion is noticed
Tongue - red in colour
Neck- no swellings noticed
Skin - Multiple hyper pigmented macules seen all over face, upper limbs, neck, thigh, abdomen and upper back.Thickening of skin over forearms, dorsum of hand and fingers and on and around mouth.
Slight peeling is still present over the arms and legs.
SYSTEMIC EXAMINATION
Respiratory system
Inspection :
Trachea : central in position
Shape of chest: bilaterally symmetrical
Movements of chest wall : decreased on left side compared to right side.
Palpation:
Trachea: central
Apex beat : located at 5 th intercostal space at midclavicular line
Chest expansion : decreased on left side
Vocal fremitus : decreased in inframammary and infra scapular region of left side
Percussion:
Dull note heard in left mamary area and ISA area.
AUSCULTATION:
Decreased air entry on left ISA,IMA area. Right side - normal air entry.
Bilateral vesicular breathing noted. Tubular breathing heard on right inter-scapular area.
coarse crepitations - end inspiratory - no variation with cough - heard on left ISA >>right ISA.
Cardiovascular system
S1 , S2 heard
No murmurs
Abdominal examination
INSPECTION:
Shape – normal
Umbilicus – Central, inverted
Flanks – free
Skin- no sinuses, striae are seen
Dilated veins – absent
Movements of the abdominal wall with respiration is present
No visible gastric peristalsis and no visible pulsations.
Palpation:
No local rise of temperature and no tenderness
No organomegaly
Percussion:
Dullness over spleen and liver
Ausculation:
Bowel sounds heard.
CNS
No focal neurological deficits
Power of muscles
Lower limb
Right. Left
Iliopsoas. 4/5. 4/5
Gluteus. 3/5. 3/5
Quadriceps. 4/5. 4/5
Hamstrings. 4/5. 4/5
Iliopsoas and quadriceps in dorsal position
Gluteus and hamstrings in prone position
Provisional diagnosis :
Systemic sclerosis
Miliary TB
Dysphagia secondary to ATT induced SJS?
INVESTIGATIONS
RBS: 70mg/dl
HbA1c : 6.8%
RFT:
Blood Urea: 136mg/dl
S. Creatinine: 4.8mg/dl
Na 139
K 3.0
Cl 102
HEMOGRAM:
HB 7.2
TC 15,000
MCV 80.4
PCV 21.5
MCH 27.0
MCHC 33.6
PLT 3.67
RDW 62
Peripheral smear - NORMOCYTIC, NORMOCHROMIC
Serum iron : 45ug/dl
ABG:
pH 7.34
PCo2 18.8
PaO2 92.4
HCO3 12.2
SpO2 96
LFT:
TB 2.8
DB 0.74
AST 14
ALT 10
ALP 673
TP 7.4
ALB 2.23
CUE:
ALB ++
Sugars nil
Pus cells plenty
Epithelial cells 1-2
COVID-19 RAT - NEGATIVE
ESR - 180
CRP - POSITIVE (1.2 mg/dl)
RA FACTOR - NEGATIVE .
LDH - 326 IU/L
Findings:
Both lungs are studded with tiny nodular densities - miliary TB or ILD?
Small air filled cyst noted left lower lobe
CXR
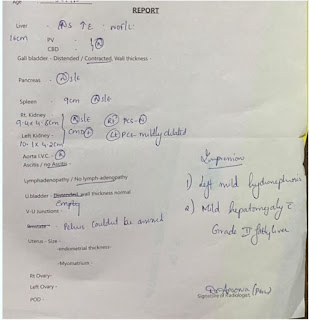
USG
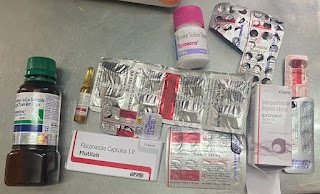
TREATMENT
Tab. Rifampicin 600mg PO OD
Tab. Isoniazid 300mg PO OD
Tab. Ethambutol 900mg PO OD
Neb. Budecort BD
Tab. Pulmoclear PO BD
Tab. Amlong 5mg PO OD
Tab. Thyronorm 50mcg PO OD
Tab. Benadon 40mg PO OD
Protein powder 1scoop + glass milk PO BD
Liquid paraffin all over the body
Mucopain gel
Inj. HUMAN ACTRAPID (only when glucose levels are high)
References:
https://venkata-phaneendra.blogspot.com/2022/03/a-50f-with-sob-since-20-days.html
https://swathi162.blogspot.com/2022/03/50-year-old-female-with-dysphagia-under.html?m=1
https://youtu.be/5DOd-y-rIBM


















Comments
Post a Comment