22 yr old male with pain abdomen
Short case
1701006104
This is an online E log book to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs
CONSENT : An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references.
M.Rambai
1701006104
CASE
My case is of a 22 yr old male ,painter by occupation ,came with chief complaints of pain abdomen since 4 days .
HISTORY OF PRESENT ILLNESS
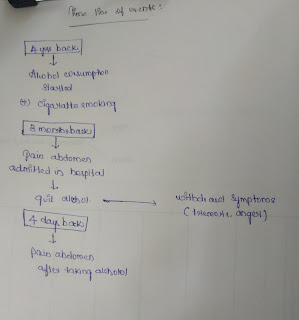
Patient started taking alcohol from the age of 18 years , reason for starting alcohol was due to peer pressure ,and later it began as addiction .
He also has habit of smoking cigarettes ,he used to smoke 5 cigarettes per day .
Then ,3 months ago he developed pain abdomen which was insidious in onset, dragging type and aggravated on standing , eating food and relived on forward bending and lying down .
He went to hospital and was advised to quit alcohol ,so he stopped consuming alcohol .
But he developed alcohol withdrawal features like excessive anger,tremors ,and cravings for alcohol .
4 days back ,he had a fight with his wife and so took alcohol again .
After which ,he had pain abdomen ,but didn't tell to his family members.
In view of his withdrawal symptoms he brought to psychiatry department for de addiction ,and then he said about his pain abdomen ,for which he was referred to medicine department and admitted.
PAST HISTORY
H/o similar complaint in past 3 months back.
No h/o previous medical, surgical history.
FAMILY HISTORY
Not significant
PERSONAL HISTORY
Diet : mixed
Appetite : normal
Bowel bladder: regular
Sleep: inadequate
Addictions - alcohol consumer,stopped 3 months back .
GENERAL EXAMINATION
Pateint is conscious , coherent and cooperative
Well oriented to time place and person
Thin built and moderately nourished .
Pallor - absent
No icterus,cyanosis , clubbing,lymphadenopathy, edema
Patient has Ryles tube connected
VITALS
Temperature- afebrile
Pulse rate- 94bpm
Blood pressure-120/80mmHg
Respiratory rate- 16cpm
SYSTEMIC EXAMINATION
ABDOMINAL EXAMINATION
INSPECTION
Shape of the abdomen- flat
Umbilicus is central
No visible scars,pulsations, peristalsis, engorged veins
PALPATION
All the inspectory findings are confirmed.
Tenderness present over the epigastrium and left hypochondrium region
No local rise of temperature
Liver - palpable 2cms below costal margin
Liver span: 11.5cm ( normal)
Spleen : not palpable
PERCUSSION
No free fluid
AUSCULTATION
Bowel sounds heard
RESPIRATORY SYSTEM
Bilateral air entry present
Normal vesicular breath sounds
no added breath sound
CVS :
S1 S2 heard
no added murmurs
CNS :
Higher mental functions- intact
No motory and sensory deficit.
Cranial nerves normal
INVESTIGATIONS
Lipase levels
Blood grouping
Blood sugar
RFT
USG
PROVISIONAL DIAGNOSIS
Pseudocyst of pancreas
TREATMENT
*Nil per oral
*IV fluids - Ringer lactate ,Normal saline 100 ml per hour
*Inj. Tramadol100mg in 100ml NS IV BD
*Inj.pantop 40 mg IV OD
*Inj. Optineurin 1 ampoule in 100ml NS IV OD
Psychiatry medication
Tab . Lorazepam 2mg BD
Tab . Benzothiamine100mg









Comments
Post a Comment